Access Menu
Our video about Venous AccessWhat is a Central Venous Access Catheter or CVAC?What happens when I get a CVAC? Will it hurt?How do I prepare for the procedure?Are there alternatives to CVACs?Can I shower after the CVAC procedure?How long will I need to have the CVAC?Are there any risks related to a CVAC?How can I avoid infections related to my CVAC?Do I always need a dressing on my CVAC?What are the signs of CVAC infection?How can I avoid blockage of my CVAC?How do I know that my CVAC is blocked?What should I do if I think my CVAC is blocked or an infection does not clear up with extra care?I know I need to call my doctor if I have an infection that does not go awaiy with care at home or if I think my CVAC is blocked. Are there other times I should call my doctor about the CVAC?Will the CVAC limit my activity?What supplies will I need to take care of my CVAC?Will the CVAC last as long as I need it?What happens when I no longer need my CVAC?
Our video about Venous Access
What is a Central Venous Access Catheter or CVAC?
A CVAC is a tube that is inserted beneath your skin so there is a simple, pain-free way for doctors or nurses to give you nutrients, or to draw your blood. When you have a CVAC, you are spared the irritation and discomfort of repeated needle injections.
Doctors recommend CVACs for patients who regularly undergo dialysis or chemotherapy treatments, or for patients who frequently receive antibiotic or antifungal infusions or nutritional supplements.
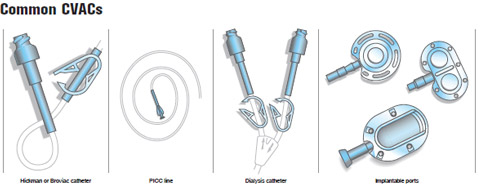
More than 3.4 million CVACs are placed each year, and doctors increasingly recommend their use. There are several types of CVACs, including tunneled catheters (you may hear them called Hickman or Broviac catheters), peripherally-inserted central catheters (sometimes called PICC lines or long lines), dialysis catheters and implantable ports. Your doctor can explain which one is best for you.
What happens when I get a CVAC? Will it hurt?
An interventional radiologist will do the CVAC procedure. You will receive medication to help you relax, and the area will be numbed. A needle is inserted into the skin, creating a small tunnel. The CVAC is then placed in the tunnel with the tip coming to rest in a large vein.You may feel some pressure and slight discomfort during the procedure, but it is not very painful.
How do I prepare for the procedure?
If you already are a patient in the hospital, your nurses and doctors will give you instructions on how to prepare for your CVAC.
If you are being admitted to the hospital on the morning of your CVAC procedure, or if you are having your procedure done as an outpatient, follow these instructions unless your doctor specifies otherwise:
Eating
Do not eat solid food after midnight on the night before your procedure. You may drink clear liquids.
Medication
Most people can continue to take their prescribed medication. If you are a diabetic and take insulin, ask your doctor about modifying your insulin dose for the day of your procedure. If you take a blood thinner, such as Coumadin, you must tell your doctor so that it can be stopped. Bring all your medications with you.
Are there alternatives to CVACs?
The alternative is to continue receiving medication or drawing blood using an IV or needle each time you undergo a procedure. If your doctor recommends a CVAC, its with your best interest in mind. A CVAC will make your frequent treatments more comfortable.
Can I shower after the CVAC procedure?
Most doctors recommend that showering be avoided until the incision heals.
How long will I need to have the CVAC?
It depends on your medical condition. A CVAC may be needed for periods from a few weeks or months to several years. Your doctor can give you more information.
Are there any risks related to a CVAC?
Placement of a CVAC is a safe procedure. The most common complications are infections, blockage of the CVAC and, occasionally, clotting of the blood. All can be resolved with appropriate medical care.
How can I avoid infections related to my CVAC?
To avoid infections, follow these instructions unless your doctor specifies otherwise:
- Keep the skin around your CVAC dry. After the incision heals, you can take showers, but cover the area with plastic wrap. Tape the edges of the plastic wrap to your skin so that water cannot get in. If the area does get wet, dry the skin completely after your shower.
- Keep the skin around your CVAC clean. Clean the area every day or every other day with a cotton swab that has been moistened with peroxide. Always wash your hands before you clean the CVAC site.
- Keep the skin around your CVAC covered. After cleaning the skin around the CVAC site, cover the area with a clean bandage or dressing. Change the dressing if it gets wet.
Do I always need a dressing on my CVAC?
It is important to keep your CVAC very clean. A dressing is usually recommended.
What are the signs of CVAC infection?
Signs of an infection are redness, soreness and swelling of the skin around the CVAC. If you notice any of these signs, even if they are very mild, follow these instructions unless your doctor specifies otherwise:
- Clean the skin around your CVAC more often. For example, if you usually clean the skin and change the dressing every other day, start cleaning the skin and changing the dressing daily. If you usually clean the skin and change the dressing once a day, do this twice a day.
- Apply antibiotic ointment to the skin around the CVAC each time you clean it.
- If your symptoms of infection improve promptly, keep up the extra care for one week. Then go back to your usual CVAC care routine. If the symptoms continue or you have questions or concerns, call your doctor.
How can I avoid blockage of my CVAC?
Sometimes, despite your best efforts, your CVAC can become blocked. To reduce the risk, flush your CVAC with sterile saline once a day. Flushing the CVAC with saline keeps the inside as clean as possible.
How do I know that my CVAC is blocked?
A sign that your CVAC is blocked is leakage of fluid near its opening or feeling resistance when you flush it. If you feel resistance when flushing, do not continue and call your doctor immediately.
What should I do if I think my CVAC is blocked or an infection does not clear up with extra care?
Call the interventional radiologist who placed your CVAC and/or your primary care doctor immediately. The doctor will arrange for proper treatment of your problem. In some cases, you will need to have your CVAC changed, and you may need antibiotic medicine. You may even need to be admitted to the hospital.
I know I need to call my doctor if I have an infection that does not go awaiy with care at home or if I think my CVAC is blocked. Are there other times I should call my doctor about the CVAC?
Yes. Call your doctor immediately if:
- your CVAC becomes dislodged or broken
- you have stitches and they become loose
- your CVAC begins to leak
- there is blood in or around your CVAC
- flushing or injecting medication causes pain
Will the CVAC limit my activity?
You will be sore for one to two weeks after your CVAC is first inserted. This will limit your activity. After that, you should continue to avoid any activity that causes a pulling sensation or pain around the CVAC. To avoid unnecessary problems, the catheter that is outside your body should be secured with tape.
What supplies will I need to take care of my CVAC?
Unless your doctor specifies otherwise, you will need to buy:
- hydrogen peroxide
- cotton swabs or cotton balls
- gauze pads
- surgical tape
- antibiotic ointment
- sterile saline
- syringes
These are available at drug stores and hospital supply stores. Your doctor will let you know if there are supplies you need that are not on this list.
Will the CVAC last as long as I need it?
Yes. Your CVAC should last as long as you need it – anywhere from a few weeks to many years.
What happens when I no longer need my CVAC?
In most situations, the CVAC will be removed. However, if you suffer from chronic, recurring problems, your doctor may choose to leave it in place.